In recent months, the U.S. Food and Drug Administration has issued emergency use authorizations (EUA) for three monoclonal antibody (mAb) therapies for the treatment of mild-to-moderate COVID 19 in non-hospitalized patients with laboratory-confirmed SARS-CoV-2 infection who are at high risk for progressing to severe disease and/or hospitalization (1). These potent mAbs are directed against the spike protein of SARS-CoV-2, blocking the virus’ attachment and entry into human cells and thereby reducing the viral load.
The three anti-SARS-CoV-2 mAb products are:
- bamlanivimab plus etesevimab
- casirivimab plus imdevimab
- sotrovimab
According to the Health Care Providers Fact Sheets (2,3,4), all three mAb therapeutics must be administered via the intravenous (IV) route (except in the case of casirivimab plus imdevimab, where subcutaneous injection is an acceptable alternate route of administration when intravenous infusion is not feasible and would lead to delay in treatment) (5).
In addition, the use of an IV in-line filter is either required or strongly recommended for all three COVID-19 mAb therapeutics.
Unfortunately, the selection of an appropriate IV in-line filter for infusing mAb used for the treatment of COVID-19 is not a trivial undertaking and identifying a suitable product can be challenging.
Statements regarding the routes of administration and the use of IV in-line filters according to the Health Care Providers Fact Sheets
| Product | Statements regarding the routes of administration | Statements regarding the use of IV in-line filters |
| bamlanivimab plus etesevimab (2) | Administer bamlanivimab and etesevimab together as a single intravenous (IV) infusion via pump or gravity. | Use of an in-line or add-on 0.2/0.22 micron polyethersulfone (PES) filter is strongly recommended. |
| casirivimab plus imdevimab (3) | REGEN-COV may be administered by intravenous infusion or subcutaneous injection. | Administer the entire infusion solution in the bag via pump or gravity through an intravenous line containing a sterile, in-line or add-on 0.2-micron polyethersulfone (PES) filter. |
| sotrovimab (4) | Sotrovimab must be administered after dilution by intravenous (IV) infusion. | Use of a 0.2 micron polyethersulfone (PES) filter is strongly recommended. |
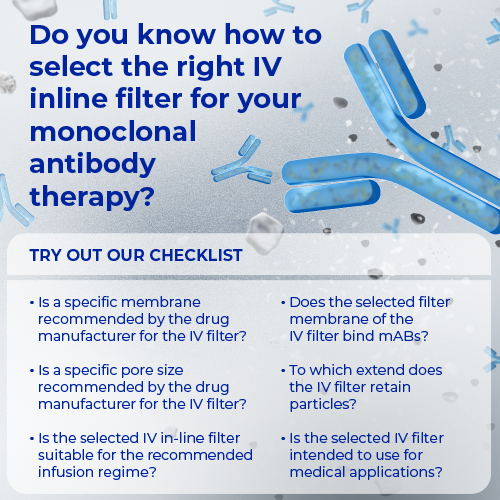
To select the right IV in-line filter, six crucial questions must be asked and answered:
- Is a specific membrane recommended by the drug manufacturer for the IV in-line filter?
- Is a specific pore size recommended by the drug manufacturer for the IV in-line filter?
- Is the selected IV in-line filter suitable for the recommended infusion regime?
- Does the selected filter membrane of the IV in-line filter bind mAbs?
- To what extent does the IV in-line filter retain particles (i.e., protect the patients from possible harmful effects of particles)?
- Is the selected IV in-line filter intended to use for medical applications?
Fact-checking: Our Supor™ AEF1 IV in-line filters
Does our AEF1 Supor™ IV in-line filter meet the drug manufacturer requirements to use a polyethersulfone (PES) membrane?
Yes. Injectable drugs may require filtration for the purpose of preparation and/or administration (6). In the case of protein-based drugs, such as mAbs, manufacturers usually recommend a low-protein binding membrane. In the case of the mAb therapeutics for SARS-CoV-2 patients, the manufacturers gave more information regarding the selection of an appropriate IV in-line filter membrane. The Health Care Providers Fact Sheets recommend the use of a PES membrane for all three mAb therapeutics.
Statements regarding the use of an appropriate filter membrane according to the Health Care Providers Fact Sheets
| Product | Statements regarding the use of an appropriate filter membrane |
| bamlanivimab plus etesevimab (2) | Use of an in-line or add-on 0.2/0.22 micron polyethersulfone (PES) filter is strongly recommended. |
| casirivimab plus imdevimab (3) | Administer the entire infusion solution in the bag via pump or gravity through an intravenous line containing a sterile, in-line or add-on 0.2-micron polyethersulfone (PES) filter. |
| sotrovimab (4) | Use of a 0.2 micron polyethersulfone (PES) filter is strongly recommended. |
Fact-checking: Our AEF1 Supor™ IV in-line filters contain a PES membrane and therefore meet the drug manufacturer requirements.
Does our AEF1 Supor™ IV in-line filter meet the drug manufacturer requirements to use a membrane with a 0.2/0.22 pore size membrane?
Yes. IV in-line filters are classified by their pore size, such as 0.2, 1.2, 5 microns (µm). The size designation gives the ability of the IV in-line filter to retain particles and organisms. The pore size required may be defined by the instructions for use of a drug or solution. The Health Care Providers Fact Sheets recommend the use of an IV in-line filter with a 0.2 or 0.2/0.22 micron pore size.
Statements regarding the use of an appropriate pore size according to the Health Care Providers Fact Sheets
| Product | Statements regarding the use of an appropriate pore size |
| bamlanivimab plus etesevimab (2) | Use of an in-line or add-on 0.2/0.22 micron polyethersulfone (PES) filter is strongly recommended. |
| casirivimab plus imdevimab (3) | Administer the entire infusion solution in the bag via pump or gravity through an intravenous line containing a sterile, in-line or add-on 0.2-micron polyethersulfone (PES) filter. |
| sotrovimab (4) | Use of a 0.2 micron polyethersulfone (PES) filter is strongly recommended. |
Fact-checking: Our AEF1 Supor™ IV in-line filters are 0.2 micron IV-line filters and therefore meet the drug manufacturer requirements.
Is our AEF1 Supor™ IV in-line filter suitable for the recommended infusion regime for SARS-CoV-2 patients?
Yes. One of the complications of therapy with mAb is the occurrence of infusion-related reactions and knowledge about the maximum tolerated infusion rate and the different ways of reducing infusion reactions while finding the right infusion rate will help to make administration of mAbs more patient-friendly (7). An IV in-line filter is an important infusion component and potential negative effects of flow rate variability must be considered (8,9). Following infusion/administration regimes are recommended for the mAb therapeutics according to the Health Care Providers Fact Sheets.
Statements regarding the appropriate administration and infusion rate and time according to the Health Care Providers Fact Sheets
| Product | Statements regarding administration | Statements regarding the infusion rate and time |
| bamlanivimab plus etesevimab (2) | Administer bamlanivimab and etesevimab together as a single intravenous (IV) infusion via pump or gravity. | The maximum infusion rate varies from 260 mL/hr to 310 mL/hr and the minimum infusion time varies from 21 to 70 minutes depending as well on the patient weight as on the size of the prefilled 0.9% sodium chloride infusion bag used. |
| casirivimab plus imdevimab (3) | Administer the entire infusion solution in the bag via pump or gravity through an intravenous line containing a sterile, in-line, or add-on 0.2-micron polyethersulfone (PES) filter. | The maximum infusion rate varies from 165 mL/hr to 310 mL/hr and the minimum infusion time varies from 20 to 49 minutes depending as well on the dose of casirivimab and imdevimab as on the size of the prefilled 0.9% sodium chloride or 5% dextrose infusion bag used. |
| sotrovimab (4) | Do not administer as an IV push or bolus. | Administer the entire infusion solution in the bag over 30 minutes. |
Fact-checking: Our AEF1 Supor™ IV in-line filters are compatible with all standard clinical infusion administration sets, including use with infusion pumps and gravity infusions and meet the requirements for the recommended infusion regime for the mAb therapeutics for SARS-CoV-2.
Does our AEF1 Supor™ IV in-line filter bind mAbs?
Binding or adsorption of mAbs to an IV in-line filter membrane may lead potentially to drug loss. To minimize this risk, we evaluated the compatibility of our AEF1 Supor™ IV in-line filters containing a 0.2 µm low protein binding Supor™ membrane with immunoglobulins (IgG) (10). Two typical monoclonal antibody drug administration scenarios were simulated by infusion of radiolabeled IgG in saline. The results of this study demonstrated that “with a full clinical evaluation, Cytiva Supor™ AEF1 in-line filters can potentially be used during infusion of monoclonal antibody-based drugs.”
Further, B.P. Werner investigated the protein recovery rate of 19 biopharmaceutical products, including mAbs with a variety of filters, including our AEF1 Supor™ IV in-line filter (11). Overall, protein recovery after filtration was very high in most cases, and protein adsorption was also not noted for filters with a diameter of 25 mm or 28 mm. Werner concluded that protein adsorption on the filter membrane will be negligible for high dosed antibodies. Table 1 illustrates the protein adsorption effectiveness of our AEF1 Supor™ IV-inline filter with MabThera, which was the first therapeutic mAb to target cells that have the CD20 marker on their surface.
Table 1. Protein adsorption as determined by high-performance size exclusion chromatography (11)
| Product | Before filtration | AEF1 IV in-line filter |
| MabThera 100 mg (1.5 mg/mL) | 100 ± 1.25 | 98.59 ± 0.78 |
| MabThera 100 mg (1.5 mg/mL) – stir stress | 100 ± 1.61 | 98.36 ± 1.58 |
| MabThera 100 mg (4 mg/mL) | 100 ± 0.64 | 99.94 ± 0.56 |
Fact-checking: Our Supor AEF1 Supor™ IV in-line filters can potentially be used for the infusion of mAb drugs without drug loss, including mAb therapeutics for SARS-CoV-2.
Does our AEF1 Supor™ IV in-line filter retain particles?
Yes. Protein formulations, such as mAb formulations, include the risk and potential for proteinaceous particles, especially when product design such as formulation, manufacturing process unit operations, or packaging/device are not fully optimized. Such proteinaceous particles have been hypothesized to provide some risk for unwanted immunogenicity, and hence industry typically aims to reduce these proteinaceous particles (11). Hence, IV in-line filters should have the capability to diminish particles effectively of all sizes, from small 1 µm particles to large 25 µm particles. In this regard B.P. Werner analyzed the filtration effectiveness of a variety of filters, including our AEF1 IV in-line filter. All filters in his study were able to diminish the number of particles.
Fact-checking: Our AEF1 Supor™ IV in-line filters retain particles.
Is our AEF1 IV in-line filter intended to use for medical applications?
Yes. Not all filters on the market are intended to use for medical applications, besides their potential effectiveness in retaining particles, low protein binding performance, and meeting the requirements of the drug manufacturer regarding type of the membrane and pore size. B.P. Werner also analyzed our Acrodisc™ and PharmAssure™ filters. Both are syringe filters. PharmAssure™ is registered for medical applications but mainly for use in pharmacy to prepare drugs, whereas Acrodisc™ is only for laboratory applications (11).
Fact-checking: Our AEF1 Supor™ IV in-line filters are intended to use for medical applications.
Summary
An increasing number of monoclonal antibodies is already available or in the process of being approved for the treatment of COVID-19 patients. These drugs have been issued with clear recommendations regarding filtration. Treating clinicians and pharmacists should be aware of the differences with filtration devices and check with our Scientific and Laboratory Services (SLS) and/or our Clinical Specialist team for more information.
Our AEF1 Supor™ IV in-line filters tick all 6 boxes and is our recommendation for filtering the new monoclonal antibody treatments for SARS-CoV-2 patients.
The products advertised within this blog are CE marked under the Medical Devices Directive (93/42/EEC) and FDA 510k registered. Please check with the local Cytiva office for availability.
MabThera is a trademark of F. Hoffman La Roche AG. REGEN-COV is a trademark of Regeneron Pharmaceuticals, Inc. Any other third-party trademarks are the property of their respective owners.
References
- United State Food and Drug Administration (U.S. FDA). COVID-19 Treatment Guidelines. Anti-SARS-CoV-2 Monoclonal Antibodies. https://www.covid19treatmentguidelines.nih.gov/therapies/anti-sars-cov-2-antibody-products/anti-sars-cov-2-monoclonal-antibodies/. Updated [2022 Dec 28]. Accessed [2021 Aug 4].
- Eli Lilly and Company. Fact Sheet For Health Care Providers Emergency Use Authorization (EUA) of Bamlanivimab and Etesevimab. A2.0-ETE-NL0007-EUA HCP-20211222. Accessed [2021 Sep 16].
- Regeneron Pharmaceuticals, Inc. Fact Sheet For Health Care Providers Emergency Use Authorization (EUA) Of Regen-Covtm (Casirivimab And Imdevimab). REC.22.01.0022. Revised [2022 Jan]. Accessed [2021 Sep].
- GlaxoSmithKline LLC. Fact Sheet For Healthcare Providers Emergency Use Authorization (EUA) Of Sotrovimab. STR: XPS. Revised 2022 Mar].
- Regencov. January 24, 2022: REGEN-COV Usage Revisions. Accessed [2021 Sep].
- Ipema HJ, Zacher JM, Galka E, Nazari J, Varabyeva A, Yu M, et al. Drugs to Be Used With a Filter for Preparation and/or Administration-2019. Hosp Pharm. 2021;56(2): 81-87. doi:10.1177/0018578719867660.
- Rombouts MD, Swart EL, VAN DEN Eertwegh AJM, Crul M. Systematic Review on Infusion Reactions to and Infusion Rate of Monoclonal Antibodies Used in Cancer Treatment. Anticancer Res. 2020;40(3):1201-1218. doi:10.21873/anticanres.14062.
- Chau DF, Vasilopoulos T, Schoepf M, Zhang C, Fahy BG. Syringe Pump Performance Maintained with IV Filter Use During Low Flow Rate Delivery for Pediatric Patients. Anesth Analg. 2016;123(3):705-714. doi:10.1213/ANE.0000000000001273.
- Jonckers T, Berger I, Kuijten T, Meijer E, Andriessen P. The effect of in-line infusion filtering on in-line pressure monitoring in an experimental infusion system for newborns. Neonatal Netw. 2014; 33(3):133-137. doi:10.1891/0730-0832.33.3.133.
- Saunders D, Stenning M. Technical Report: Binding of Monoclonal Antibodies to Pall Supor™ AEF1 Intravenous Filters. Pall Life Sciences. 210112.1IGL. Published [2021].
- Werner BP, Winter G. Expanding Bedside Filtration-A Powerful Tool to Protect Patients From Protein Aggregates. J Pharm Sci. 2018;107(11): 2775-2788. doi:10.1016/j.xphs.2018.07.022.
Author bio
Dr. Volker Luibl, MBA

Dr. Luibl is a Demand Generation Marketing Manager with knowledge in medical device and clinical science.